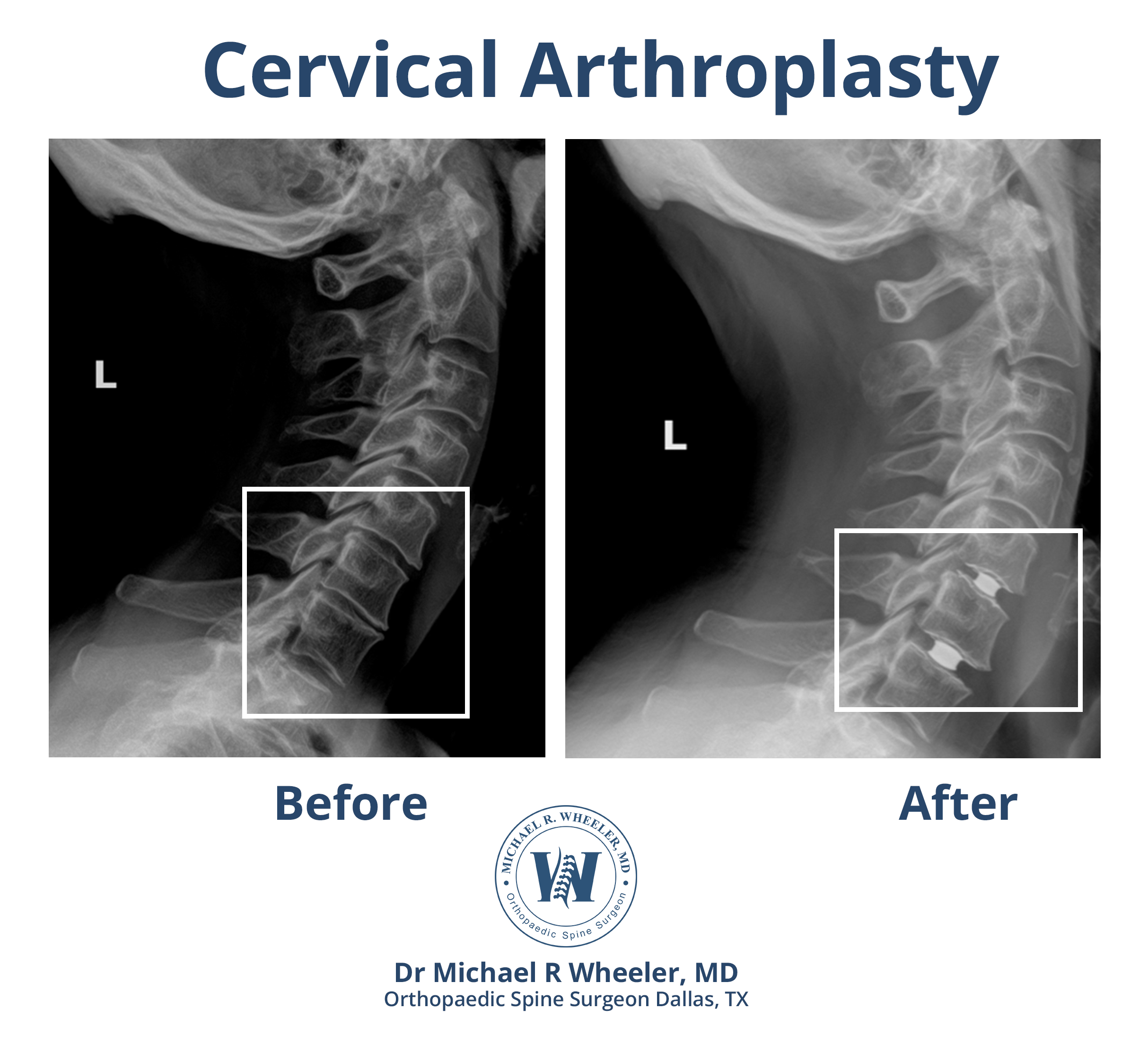
Discs in the cervical spine (or neck) can degenerate over time or herniate, causing pressure on the spinal cord or the exiting nerve roots. This can lead to neck pain and/or pain, weakness, numbness, or tingling of the shoulder, arm, or hand on the affected side. Cervical disc replacement is a surgical procedure used to take the pressure off affected nerves by removing the herniated or degenerated disc of the cervical spine and replacing the diseased disc with a new artificial disc.
During this procedure, an incision is made in the front of the neck to remove the diseased disc. Depending on the number of problematic discs, one or more discs may be removed. Once the disc(s) is removed, an artificial disc is placed in the space between the vertebrae. This is a motion-preserving procedure and is an alternative to a fusion.
Benefits of Cervical Disc Replacement
- Relief of arm and shoulder pain caused by pinched nerves in the neck
- Relief of weakness, numbness, or tingling of the arms caused by pinched nerves in the neck
- Relief of neck pain due to degenerative discs in the neck
- Preserves motion of the neck
Patients who would benefit from cervical disc replacement
- Patients who have neck pain because of degenerative or herniated discs of the neck
- Patients with shoulder/ arm weakness, pain, numbness, or tingling due to pinched nerves of the neck that have failed conservative treatment
- Patients without significant arthritis in the joints of the spine
- Patients without significant alignment problems of the spine
Procedure
Positioning: The patient is positioned supine (on his or her back). General anesthesia is used for this surgery.
Neuro monitoring set up: Advanced monitoring of the nerves and spinal cord is used throughout the entire surgery that allows for safe monitoring of each nerve and its function.
Incision: A small incision is made on the front of the neck.
Exposure: The muscles and blood vessels of the neck are carefully moved out of the way to allow access to the spine.
Identifying the affected level: X-ray is used to confirm the appropriate surgical level.
Disc removal: The diseased disc and any bone spurs are removed.
Decompression: Once the disc has been removed, the pressure is taken off the spinal cord and nerves using direct visualization.
Disc replacement trial: Different sized artificial discs are trialed in the disc space to ensure the proper fit for each individual patient.
Placement of the artificial disc: The selected artifiticial disc is carefully placed between the vertebrae. X-ray is used to confirm adequate positioning of the disc.
Incision closure: The incision is closed with absorbable suture and a dressing is placed.
Risks and complications associated with cervical disc replacement
Although risks associated with cervical disc replacement are rare, patients undergoing this surgery should be aware of the risks involved and discuss the following with the surgeon prior to surgery:
- Hoarseness – this is usually temporary and usually resolves within a few days after surgery
- Trouble swallowing – this is usually temporary and usually resolves within a few days after surgery
- Horner’s Syndrome – this is an extremely rare complication caused by damage to the sympathetic nerves
- Damage to the esophagus
- Damage to the blood vessels of the neck
- Spinal cord or nerve injury
- Pain, bleeding, infection – which are risks of any surgery
- Loosening of implanted artificial disc
Recovery
- Patients usually wake up from surgery with immediate relief of arm or shoulder pain.
- Depending on the number of surgical levels, the patient may discharge home the same day of surgery.
- Complete recovery from surgery varies from patient to patient, but patients can usually return to normal activities 6-12 weeks after surgery.
Cervical disc replacement vs ACDF
Cervical disc replacement is an alternative surgery to anterior cervical discectomy and fusion (ACDF). Both surgeries are excellent procedures designed to treat similar problems. There are subtle differences that make one surgery preferential over the other depending on the patient’s symptoms, imaging, goals, age, etc. The decision regarding which surgery is best for the individual patient should be discussed with the surgeon.